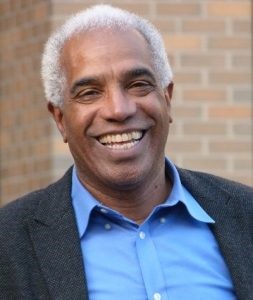
COVID-19 poses many challenges — particularly to vulnerable populations such as older adults — but with every challenge is an opportunity to overcome it. We spoke with Dr. John K. Holton, PhD., to discuss lessons learned and positive outcomes during the pandemic. Holton is Director of Strategic Initiatives for Social Policy and Research at the Jane Addams School of Social Work at the University of Illinois at Chicago and board member at Sage Collective.
Finding New Ways to Connect
With older adults at higher risk of being severely affected by COVID-19, many are taking CDC safety guidelines more seriously than the average American, which can lead to increased social isolation and loneliness. “While no one is happy to see the quality of life for older adults affected,” explains Holton, “increased awareness of the risk of social isolation has created a positive impact: people are now more concerned about the wellbeing of older adults than ever before.”
The increased attention and care for older adults in our communities has led to inventive, highly organized solutions. “We’ve seen responses raised, like setting up phone banks or block-by-block check-ins on homes led by local faith institutions,” says Holton. “These solutions are being used to blanket communities with networks that were always there informally, but that have now taken on a more formal responsibility of influence.”
Holton goes on to say: “During the pandemic, the slogan we’re all in this together has arisen. But what should go hand-in-hand with that slogan is the additional call to action: and here’s how you can be helpful. That kind of thinking is what takes the spirit from passive connection to fruitful action, making the power of the collective come alive.”
Making Solutions Accessible
Every challenge (and subsequent solution) is a learning experience. Holton echoes this sentiment: “There are lessons we’re learning from experiencing this pandemic, and best practices we’re evolving for the years to come, because while this is the first pandemic in over a hundred years, it certainly won’t be the last, and we need to be prepared. We’re gaining invaluable understanding and insight as we go, as this pandemic continues to reshape our economy and our social practices.”
But as we invent new solutions, they can’t be one size fits all. Different circumstances call for different approaches, and Holton stresses the importance of accessibility and consideration for more vulnerable populations (such as older adults). “In other words, as we develop best practices writ large, are we making sure to adapt them to apply to our most vulnerable populations?” challenges Holton.
Learning Lessons, New and Old
One example Holton uses is the 1995 Chicago heat wave. Over a period of five days, 739 heat-related deaths occurred in the city, with the majority of victims being elderly residents. Many could not afford air conditioning or were unable to open windows in their homes, and as a community we failed to check in on them and ensure their needs were being met. “That was a wake-up call for everybody,” reflects Holton, “including city government. We knew then we had to do better. Failing to meet that challenge led to posthumous solutions like cooling stations and phone banks organized by the Illinois Department of Human Services [IDHS]. In these periods of extended crisis, we learn to create solutions that fit the needs of our most vulnerable populations, because we have to, to do better as a public body.”
Another example comes from widespread criticism of the Federal Emergency Management Agency (FEMA) response after Hurricane Katrina hit in 2005. Many felt FEMA did an inadequate job of encouraging evacuation in target areas before the hurricane hit. “What we learned from FEMA,” explains Holton, “is that the protocols it had in place to help people understand the urgency of the situation only worked for a certain class of folks — in other words, folks who had transportation and were able to organize belongings and jump in their cars. Meanwhile, folks who weren’t in that position needed other types of assistance to help them evacuate. Borrowing from that example, we learned then and will learn now what does and doesn’t work with certain pockets of our population.”
We’re facing parallel challenges today: meeting the needs of nursing homes and skilled care facilities during the pandemic. Early on, many were hit hard and were scary places to be for vulnerable populations. But as time goes on and we learn more, communities are taking more civic responsibility for the health and safety of each and every person, because as Holton says, we’re all in this together, and we need to do what we can to help. And when we do work together for a better future, wonderful things arise from it.