Chicago COVID-19 Vaccination: Where We’re At Now
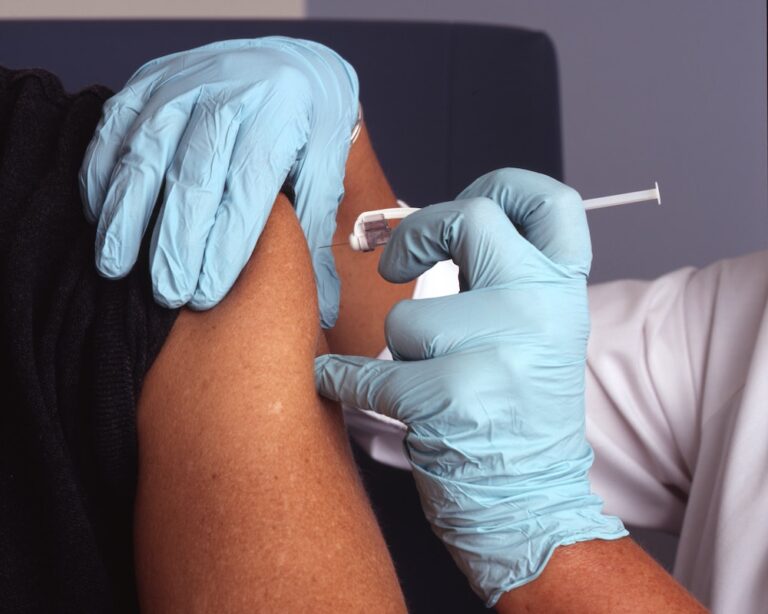
Earlier this year, we shared a blog post on what to know about the COVID-19 vaccine. Now that vaccine rollouts have been occurring nationwide, one of the biggest hurdles outside of deployment is ensuring that we, the people, feel informed and equipped with the necessary tools and knowledge to make decisions about our own vaccination. In support of that, today we’re providing an update on COVID-19 vaccination in Chicago, and where things stand now:
Understanding the State’s Phased Rollout
Illinois is administering vaccinations in a phased rollout plan — you can read the state’s comprehensive coverage of its vaccine distribution phases here. As of January 25th, Illinois entered Phase 1B: Frontline Essential. This phase made the vaccine available to all non-healthcare residential settings and Chicagoans age 65 and older.
According to Chicago, all non-healthcare residential settings includes homeless shelters, women’s shelters, adult day care programs, correctional settings (jail officers, juvenile facility staff, workers providing in-person support, detainees), and other non-health care residential settings that have experienced outbreaks (e.g. convents).
But as of February 25th, Illinois progressed further into Phase 1B Plus. This extended phase includes people (16 years of age and older) with certain underlying conditions and comorbidities. The list of conditions includes cancer, COPD (Chronic Obstructive Pulmonary Disease), diabetes, heart condition, immunocompromised state from a solid organ transplant, obesity, pregnancy, pulmonary disease and sickle cell disease.
However, it is important to note that Chicago will NOT be joining the rest of Illinois in progressing to Phase 1B Plus at this time. Due to the city’s population density, more than 95,000 Chicago residents would become eligible if we were to expand under the state’s guidelines. Therefore, the city has decided to hold off on progressing to this next stage until it is able to more fully serve those who fall into the initial Phase 1B.
Looking at Current and Future Benchmarks
According to the Illinois COVID-19 vaccine tracker, as of Wednesday, February 24th: 28,626 additional people have been fully vaccinated for a total of 619,480 — 4.86% of the state’s population.
As of that same date, 5% of all White Illinoisians have been fully vaccinated, 2% of all Hispanic Illinoisians have been fully vaccinated and 2% of all Black Illinoisians have been fully vaccinated. Chicago is seeing similar disparities: as of that same date, 6% of all White Chicagoans have been fully vaccinated, 2% of all Hispanic Illinoisians have been fully vaccinated and 3% of all Black Chicagoans have been fully vaccinated.
You can stay up-to-date on the state’s vaccination rates here.
Looking ahead: according to Governor J.B. Pritzker, Illinois expects to begin administering an average of 100,000 doses of the COVID-19 per day by mid-March.
Stay tuned for more COVID-19 vaccination updates and insights from Sage Collective.